Understanding the role of an ECLO
Posted: Monday 01 July 2024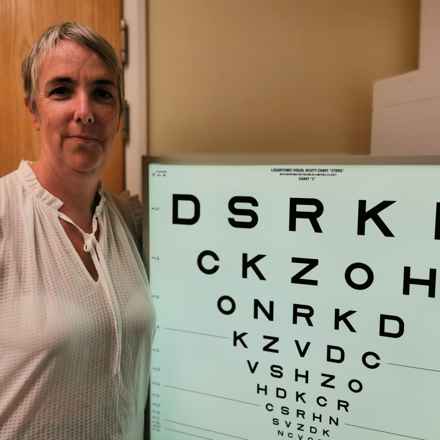
Navigating a diagnosis of macular disease can be overwhelming, but Ruth Rhydderch, an eye clinic liaison officer (ECLO) at the University Hospital of Wales, explains how her role can make a difference.
“Many people think I handle appointments and surgeries,” Ruth said, “but my role is about guiding patients through their diagnosis and connecting them to the right support.”
In our recent webinar Ruth told us more about how an ECLO can help.
What does an Eye Clinic Liaison Officer do?
An Eye Clinic Liaison Officer (ECLO) plays a pivotal role in helping and supporting patients in eye clinics. But, Ruth admitted the title can be confusing. "It's a bizarre title, isn't it? Because everyone thinks, as a liaison officer, I can book their appointments and arrange their surgery and all sorts of weird and wonderful things. But that's actually nothing to do with the role whatsoever.”
Explaining what the role of an ECLO involves, Ruth said: "I'm the sort of hub with lots of spokes to lots of different places to make sure that the patients get linked up to all the right support services."
Why is the role of an ECLO important?
Ruth said often eye clinics can be overwhelming for patients. Having an ECLO to help patients navigate the system can be helpful.
“If you're getting a load of information thrown at you,” she said. “It can be tricky to take it all on board." Ruth's role involves translating complex medical information into plain, simple language, making it accessible for patients. "I need to demystify stuff and put things in plain, simple English for people," she said, which can significantly ease the patient experience.
How does an ECLO help patients understand their condition?
Ruth said: "You see people having light bulb, penny drop moments. When something that maybe has been going on for months or years finally makes sense to them."
Giving just one example of how she talks to patients about wet age-related macular degeneration (AMD), she said: “The best analogy I've ever heard, and it's the one I use, is that it's like a leaking pipe behind a wall.”
She added: “Because just like a leaking pipe behind a wall, you can't see the leak, but the damage is occurring, and you can only see it when it's too late.
“It helps patients visualise the problem better because they can relate to the idea of a hidden leak causing damage."
Why should I contact an ECLO?
Ruth recommended anyone attending an eye clinic, who has questions or concerns, should ask about speaking to an ECLO.
She said: "I would always say to anybody who comes to an eye clinic and they're worried or they've got questions or they've got concerns, ask to speak to the ECLO."
She added: “If you've already been in touch with one or you know where yours is, don't ever sit at home worrying about things."
What if my clinic doesn’t have an ECLO?
Not all clinics have ECLOs, to find out if there is one based in your clinic patients can contact the RNIB helpline, which maintains a list of ECLOs across the country.
But, if there is no ECLO service in your clinic Ruth highlighted there is still plenty of support available.
Ruth said: "I think the best bet would be is if you can contact, if you can, your local social, adult social services, and ask them, do they have a sensory team? The answer should be yes. And also, is there a local society, is there somebody locally that supports people with vision impairment? You can also contact the Macular Society or RNIB."
What are the main questions people ask you?
The most common question people ask, according to Ruth, is about having trouble reading due to their sight loss. She said: "Whenever I talk to people about solutions, I always tell them the sorts of solutions that we tend to lead people to. And point them in the direction of really simple, small, straightforward solutions."
The other big question Ruth said she gets from macular patients, is ‘am I going to go blind?’
Dealing with this question Ruth said: “We have to have a conversation around sort of on a very basic level, what do they mean by blind? Because for most of my patients, they have a huge fear that they will wake up and all of their vision will have gone.”
What are the daily challenges people with macular disease face?
"People say to me, ‘oh, it's silly that I'm moaning about this, but, I get up in the morning and I can't make myself a cup of tea without spilling it everywhere and making a right old mess and scolding myself and I'm running into all sorts of bother with that’.”
She added: “And I've always said to people, there is nothing too small, too trivial that isn't worth at least looking at and talking about."
Advice to anyone newly diagnosed
Offering her advice to anyone newly diagnosed Ruth said:
Stay positive
“Try to stay positive. There are lots of aids and adaptations that can help maintain your independence.”
Seek out information
“Don’t be afraid to ask questions and seek out information. Understanding your condition and what to expect can help you feel more in control.”
Find support
“Lean on your support networks. Whether it’s family, friends, or support groups, having people to talk to and share your experiences with can be really beneficial.”
Stay active
“Staying active and engaged in activities you enjoy is important. It helps maintain your overall well-being.”
Watch the webinar in full
Would you like further advice or information on living with macular disease?
Get in touch by calling our helpline on 0300 3030 111.
Macular Society Helpline
Free information and support to those with macular disease, along with their family and friends, to help people retain their independence.
Who’s who in eye care
The health care system can be difficult to navigate and you might not know who to speak to, to get the right help. Understand the key roles in eye care, from optometrists to ECLOs, and who can help.