Creating a blood test to detect early AMD

Professor Majlinda Lako, Newcastle University - £229,411
March 2021 – June 2024
Background and project history
Previous research led by Professor Lako at Newcastle University developed a cell model of age-related macular degeneration (AMD) by turning patient skin cells into retinal pigment epithelium (RPE) cells, a key layer in the macula.
One of the main jobs of the RPE is producing, degrading and transporting proteins that are essential for our vision. If the RPE cells die or get damaged, as seen in AMD, it can cause light-sensing cells (photoreceptors) to die, which is what leads to sight loss.
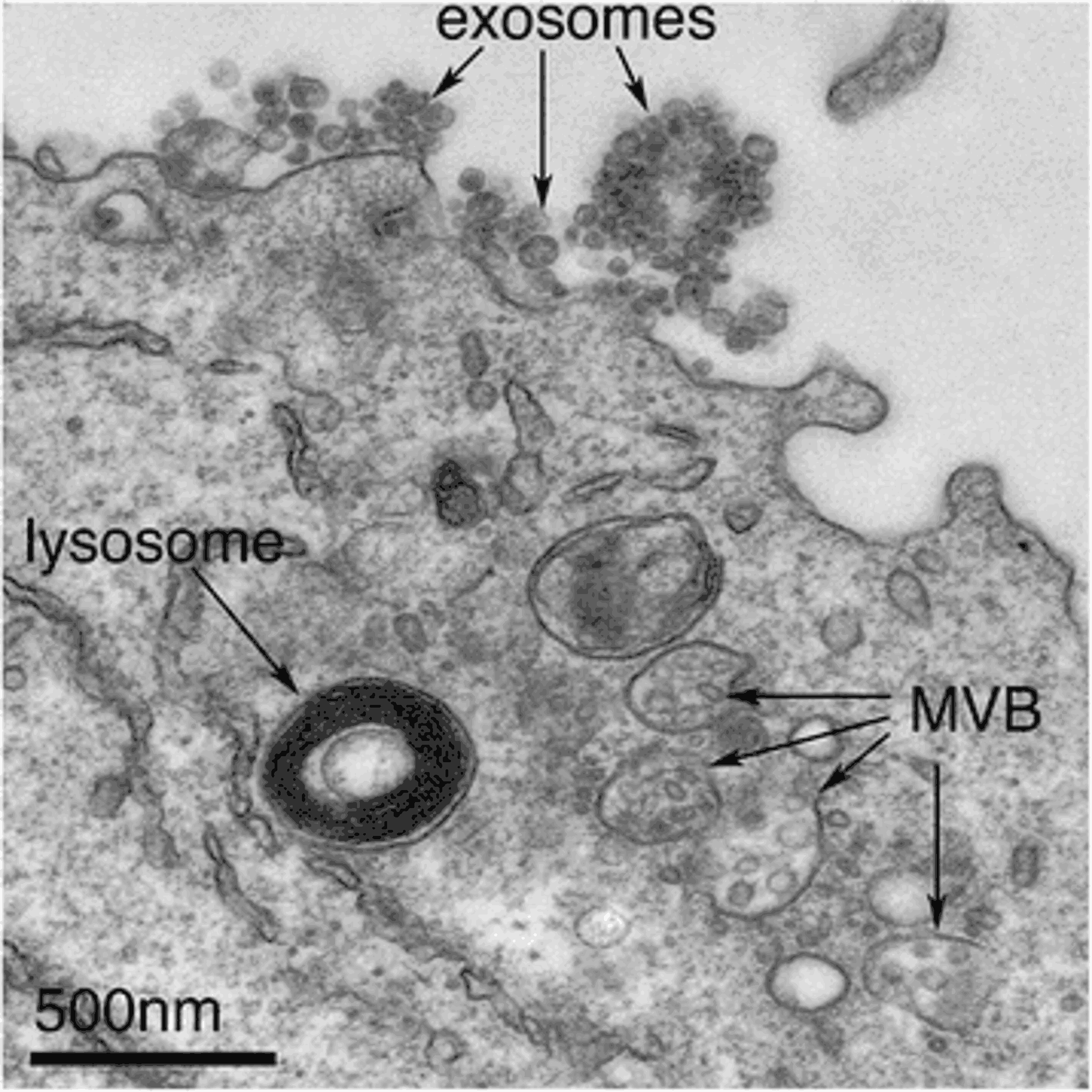
This previous project by Professor Lako, also funded by the Macular Society, found some molecules that are more abundant in AMD cells compared to healthy cells. These molecules are produced by the RPE and move outside the cells in tiny bubble-like structures, known as exosomes, which help cells to communicate with each other. When AMD is present, the RPE exosomes can potentially be harmful for the photoreceptors.
What did the researchers do?
This follow-up project aimed to further understand the role of these RPE exosomes in AMD and the proteins they contain. It looked at why they form, what they do and if they cause harm to photoreceptors. The researchers also wanted to find out if these exosomes could be detected in blood, which could help early diagnosis of AMD.
To do this, they assessed large numbers of blood and eye fluid samples from people with dry AMD and wet AMD, as well as healthy people. In doing so, the researchers were able to determine a set of proteins consistently present in AMD.
They also studied the communication between the RPE and photoreceptors via exosomes, as well as the potential toxic effect of these exosomes in cases of AMD.
What did the researchers find?
They found that RPE cells communicate with photoreceptor cells via the exosomes they produce. Having assessed the effect of these exosomes on healthy photoreceptors, they showed that in AMD, RPE exosomes cause abnormalities in the normal photoreceptor cells. This suggests they could trigger the start of macular degeneration.
Additionally, in AMD the researchers saw depleted levels of important protein building blocks, as well as dramatically fewer, and occasionally damaged cell structures required to build healthy exosomes.
Why is this important and what’s next?
Together, the findings highlight one of the potential triggers for macular degeneration and the subsequent sequence of events that lead to photoreceptor cell death and vision loss.
These important findings may lead to new treatments that could focus on stopping the production of toxic exosomes, in turn, helping to prevent the development of AMD.
Further work is still required to establish clear-cut markers that could be used to detect AMD in patients’ blood samples.
See our other projects
Since 1987 the Macular Society has invested around £10 million in over 100 research projects.
Explore more research
Beating macular disease through funding medical research and improving the lives of those living with macular disease.
Get the latest research news from the Macular Society
To hear about life-changing research and treatments, subscribe to our monthly enewsletter today. Together we can Beat Macular Disease.
Sign up to our free email newsletter